Proven Strategies to Reduce Insulin Resistance and Lose Stubborn Belly Fat Naturally
Why That Stubborn Belly Fat Won’t Budge—And What Insulin Has to Do With It
If you’re a woman over 40 and feel like your belly has suddenly become a storage zone for stubborn fat—despite eating well or exercising—you’re not imagining things. One of the biggest hidden culprits could be insulin resistance, a metabolic imbalance that becomes more common with age, hormonal shifts, and lifestyle changes.
Insulin is a hormone your body produces to help move sugar (glucose) from your bloodstream into your cells, where it’s used for energy. But as we age—especially during perimenopause and menopause—our cells can become less responsive to insulin. This means your body has to pump out more of it just to keep blood sugar levels stable. The result? Excess insulin signals your body to store more fat, particularly around the midsection.
This condition, known as insulin resistance, is often a slow-building issue that doesn’t cause obvious symptoms at first. But over time, it can lead to stubborn weight gain, low energy, sugar cravings, and even increase the risk of type 2 diabetes, heart disease, and fatty liver. It’s also closely connected to hormonal changes, making it particularly relevant for women navigating their 40s and 50s.
The good news? Insulin resistance is not permanent, and you don’t need to resort to extreme diets or punishing workouts. In fact, more gruelling exercise routines won’t help and it doesn’t address the route cause, leaving you even more frustrated. With simple, sustainable lifestyle changes—like adjusting how and when you eat, managing stress, and getting quality sleep—you can improve your body’s insulin sensitivity and finally see that belly fat start to shift.
What Causes Insulin Resistance in Women Over 40?
Insulin resistance doesn’t happen overnight—it develops gradually, often due to a combination of lifestyle, hormonal, and genetic factors. One of the biggest contributors is chronically high blood sugar, often driven by a diet high in refined carbs, sugar, and processed foods.
During my time in high pressured sales environments I was addicted to carbs to boost my energy levels. I would get that afternoon slump and fatigue and reach for a Snickers! I never really appreciated what this was doing to my body, and over time it has made me insulin resistant.
When your body is constantly working to manage glucose spikes, insulin levels remain elevated, and over time, your cells stop responding efficiently. Hormonal changes during perimenopause and menopause can also play a major role. As estrogen levels decline, the body’s ability to regulate blood sugar and store fat—especially around the belly—becomes more challenging.
Other key contributors include chronic stress, which raises cortisol (another fat-storing hormone), poor sleep, and a sedentary lifestyle, all of which reduce insulin sensitivity. Genetics can also predispose you to insulin resistance, but lifestyle habits are often the tipping point.
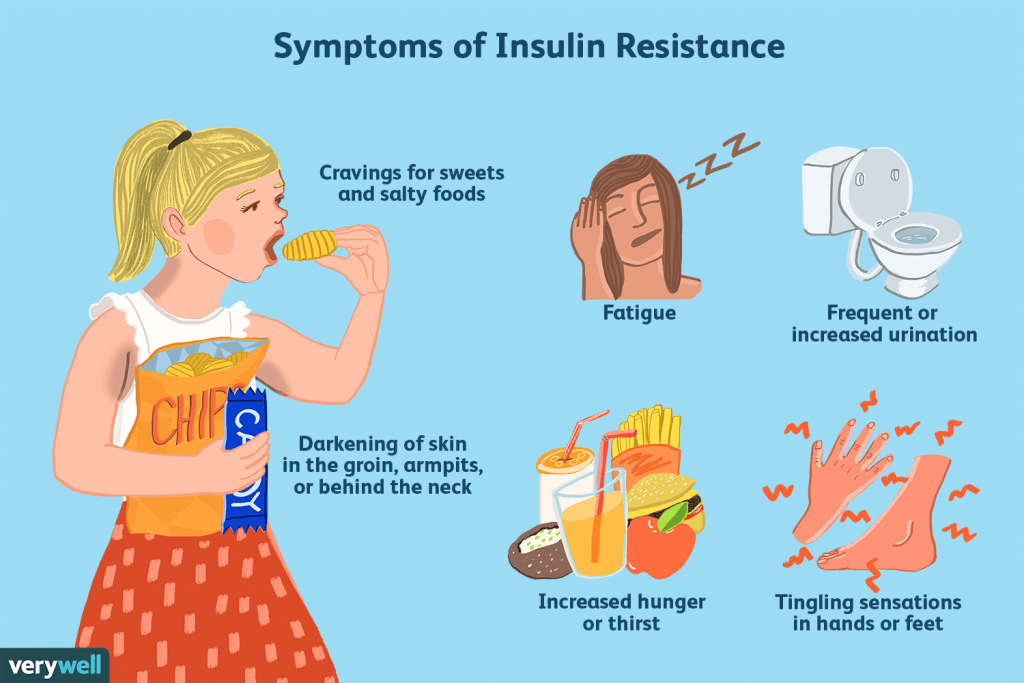
Common Symptoms of Insulin Resistance—And Why They’re Often Missed
One of the most frustrating things about insulin resistance is that it often flies under the radar—especially in women over 40—until it starts noticeably affecting your weight, energy, or mood. Many women chalk up the signs to aging or hormonal shifts, but they may actually be early red flags that your body isn’t responding well to insulin.
Here are some of the most common symptoms to watch for:
- Belly fat that won’t budge, even with exercise or dieting
- Frequent sugar or carb cravings, especially in the afternoon or evening
- Fatigue or brain fog, particularly after meals
- Increased hunger shortly after eating
- Dark patches of skin, especially around the neck, armpits, or elbows (a condition called acanthosis nigricans)
- Elevated blood pressure or cholesterol, often detected during routine checkups
- Irregular periods or signs of PCOS (in younger women), due to the hormone-disrupting effects of insulin
- Trouble losing weight, despite “doing everything right”
I’ve noticed that the fat not only sits on my belly but it also goes to my legs and thighs. I have also been diagnosed with high cholesterol and am prone to skin tags. I have fatigue after eating and get brain fog.
If you recognize several of these symptoms, it doesn’t mean something is “wrong” with you—it means your body is trying to communicate a deeper metabolic imbalance. The sooner you spot the signs, the easier it is to take action and reverse insulin resistance with supportive, sustainable changes.
How to Reverse Insulin Resistance Naturally: Tools and Tips That Work
The empowering truth is this: insulin resistance is not a life sentence. With the right daily habits, you can improve your insulin sensitivity, shrink stubborn belly fat, and feel more energized and balanced—without extreme diets or unsustainable routines. Here are the most effective science-backed strategies for women over 40:
1. Balance Your Meals with Protein, Healthy Fats, and Fiber
Start by ditching the blood sugar roller coaster. Build your meals around lean protein (like eggs, poultry, fish, or plant-based proteins), healthy fats (like olive oil, avocado, nuts), and fiber-rich vegetables. These help slow down glucose absorption and keep insulin levels steady. Limit highly processed carbs and sugars, especially in the morning.
Pro Tip: Try a “protein-first” approach to meals—starting with protein and non-starchy veggies before carbs can reduce the blood sugar spike.
2. Embrace Smart, Sustainable Movement
You don’t need to spend hours at the gym. Daily movement—even a 20-30 minute walk after meals—can significantly improve insulin sensitivity. Resistance training (like lifting weights or using resistance bands) is especially helpful for women over 40, as it builds muscle, which naturally uses glucose more efficiently.
Pro Tip: Try adding 10–15 minutes of light movement after dinner. It’s one of the simplest, most effective ways to lower blood sugar. I love going for a walk by the sea at lunch or after work, it also gives me that hit of sunshine in the day and that important red light at sunset.
3. Time Your Meals with Intermittent Fasting
Many women find success with gentle forms of intermittent fasting, such as a 12:12 or 14:10 eating window (12–14 hours fasting overnight). This gives your body time to lower insulin levels and tap into fat stores. However, fasting isn’t right for everyone—especially if it causes fatigue or stress. You can learn more about Intermittent Fasting in my post Intermittent Fasting For Menopause Belly
Pro Tip: If fasting works for you, ease into it slowly, and always prioritize nutrient-dense meals during your eating window. It is also advised to only eat when it’s light outside, although living in the UK during Winter and doing this could be a challenge!
4. Start A Healthy Keto Diet
A healthy keto diet is a low-carb, high-fat, moderate-protein eating approach designed to shift your body into a fat-burning state called ketosis—where it burns fat for fuel instead of glucose. But unlike trendy versions that focus on bacon and butter, a truly balanced keto lifestyle emphasizes whole, nutrient-dense foods like fatty fish, eggs, leafy greens, non-starchy vegetables, avocado, olive oil, nuts, and seeds.
For women over 40, this approach can be especially beneficial for managing insulin resistance, hormonal changes, and midsection weight gain—as long as it’s done mindfully. A well-formulated keto plan should also include plenty of fiber, electrolytes (like magnesium and potassium), and enough calories to support energy and hormone balance.
The goal isn’t extreme restriction, but rather to nourish your body while reducing the blood sugar spikes and crashes that contribute to fatigue, cravings, and stubborn belly fat. I will do another post on Keto soon.
5. Sleep Like It’s a Non-Negotiable
Lack of sleep increases cortisol and insulin resistance. Aim for 7–9 hours of high-quality sleep per night. Create a calming wind-down routine, keep your room cool and dark, and limit screens before bed.
Pro Tip: A magnesium supplement or herbal tea (like chamomile or lemon balm) can support more restful sleep. You can learn more in my post How To Treat Menopause Insomnia.
6. Lower Stress to Lower Insulin
Chronic stress raises cortisol, which can worsen insulin resistance and drive belly fat storage. Daily stress-reducing practices—like deep breathing, meditation, journaling, or gentle yoga—can have a powerful hormonal impact. I absolutely love my hot yoga which centres around breathwork and coming back to your centre.
According to Dr Mindy Pelz, stress, toxic thoughts and cortisol levels are the biggest factors we need to look into and heal to reduce inflammation and regulate insulin levels. With perimenopause heightening anxiety it’s even more important that we take care of our mental health.
Pro Tip: Even 5 minutes of mindful breathing or stepping outside in nature can help shift your nervous system into a calmer, fat-burning state. I have a timer on my desk that I set for 45 minutes at a time, when it goes off I move, get out into the garden or have a stretch.

7. Track Your Progress—Not Just Your Weight
Consider monitoring your waist measurement, energy levels, sleep quality, or fasting insulin/blood sugar levels (through lab work or a glucose monitor) instead of just the scale. These are more accurate markers of metabolic health and progress. You can test at home which is highly recommended so you can closely monitor it, they aren’t expensive and start from £18 on Amazon and include the testing strips.
If you are going to opt in for a Keto lifestyle then it is much better to invest in the KetMojo which monitors all of it, they have a great package deal that includes plenty of test strips and the monitor.
Pro Tip: Ask your doctor about getting your fasting insulin, HOMA-IR score, or A1C tested. These are better indicators of insulin resistance than blood sugar alone.

Final Thoughts
Understanding insulin resistance is more than just a medical journey—it’s a powerful step toward reclaiming your energy, balance, and confidence. It really can take time to digest all this information which is why I’ve provided practical steps, day by day you will see things start to shift.
It’s really woken me up to the fact that we have become so far removed from our ancestral way of being in the world. I’ve sat at a desk for 30 years and although I’ve exercised and loved movement in my life, now it’s just not enough and it’s all caught up with me. This can feel overwhelming and disheartening which is one of the reasons I started this blog, to build a community of beautiful women travelling along the same path, supporting each other.
While the process may take time, every nourishing meal, restful night’s sleep, walk around the block, and moment of stress relief is a small act of healing. Remember, your body is incredibly wise and responsive when given the right support. Whether you’re just starting to explore this path or you’re already making changes, know that you’re not alone—and every positive step counts. You deserve to feel strong, clear-headed, and vibrant in this chapter of life.
Handpicked Support for Your Midlife Journey:
Some of the links below may be affiliate links in the future. I only ever recommend products and resources I truly believe in.
🎥 Helpful Videos to Deepen Your Understanding
Your Insulin Resistance Action Plan: Simple Daily Habits to Support Hormone Balance and Belly Fat Loss
✔ Nutrition
- Prioritize protein, healthy fats, and fiber in every meal
- Minimize refined carbs and sugars, especially in the morning
- Eat protein and veggies first to reduce glucose spikes
- Consider a gentle form of intermittent fasting (12–14 hours overnight)
✔ Movement
- Move your body daily—walking, yoga, or light cardio
- Add strength training 2–3x a week to build insulin-sensitive muscle
- Take a 10–20 min walk after meals, especially dinner
✔ Stress and Sleep
- Aim for 7–9 hours of quality sleep each night
- Create a calming bedtime routine—no screens before bed
- Practice daily stress relief: deep breathing, meditation, or journaling
- Take breaks during the day to relax and reset your nervous system
✔ Hormone and Metabolic Monitoring
- Track waist circumference, energy, mood, and cravings
- Talk to your doctor about testing:
- Fasting insulin
- A1C
- HOMA-IR
- Consider using a glucose monitor/KetoMojo to track patterns
📝 Journal Prompts & Reflection Ideas
Experts I love in this field:
Candi Frazier – PrimalBod
Her Instagram page: https://www.instagram.com/theprimalbod/
Dr Mindy Pelz: Dr Mindy Pelz





Great insights on tackling insulin belly fat. I found the tips on diet adjustments and exercise really practical. For anyone interested in more women’s health guidance, I often refer to resources like SheMed’s blogs, they have some useful information.